Hepatobiliary and Pancreatic Unit
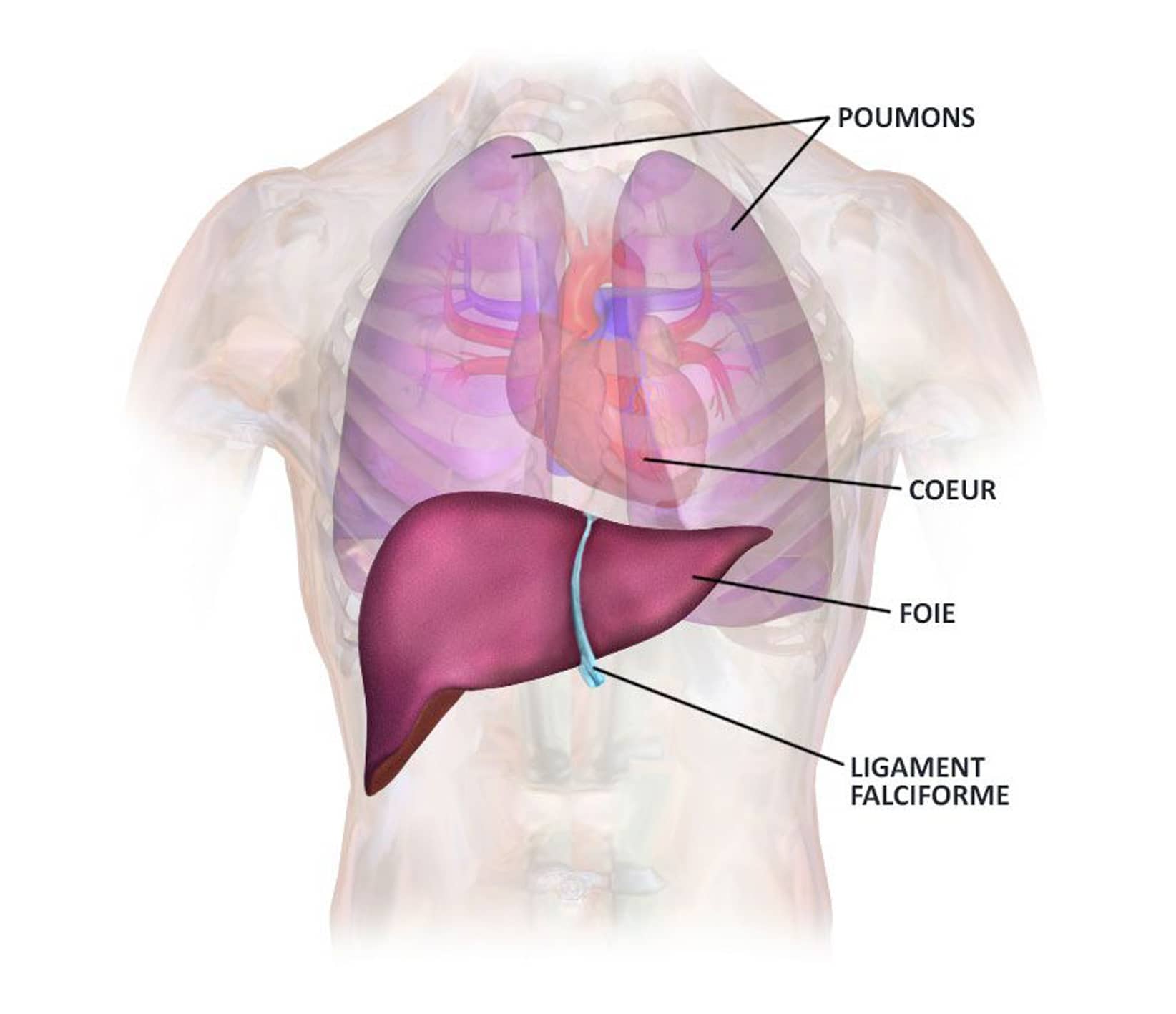
Liver anatomy
The liver is a unique abdominal organ, indispensable for life. To date, there is no way of artificially and permanently replacing its function.
It lies beneath the diaphragm, in the upper right-hand part of the abdominal cavity, and above the stomach, partly covering it. On average, it measures 28 cm wide, 16 cm high and 8 cm thick. Its own weight is approximately 1.5 kg.
The liver is a highly vascularized organ, and like the kidney, it is a great “blood cleaner”, metabolizing and neutralizing many of the toxic substances stored by the body.
The liver is a complex organ capable of remarkable regeneration, even if 3/4 of its mass has been resected or destroyed.
Hepatocellular carcinoma (HCC)
Hepatocellular carcinoma (HCC) is a primary cancer of the liver. In most cases, it is associated with cirrhosis, and is responsible for around 90% of primary tumors of this organ.
It is the 8th most common cancer worldwide. There are some 500,000 new cases worldwide every year.
In most cases, it is associated with cirrhosis and chronic infection with the hepatitis B and/or hepatitis C viruses.
In most cases, patients are asymptomatic. As the disease progresses, significant symptoms appear, such as weight loss, severe fatigue, ascites, dyspepsia, abdominal pain, hepatomegaly (large liver) and fever.
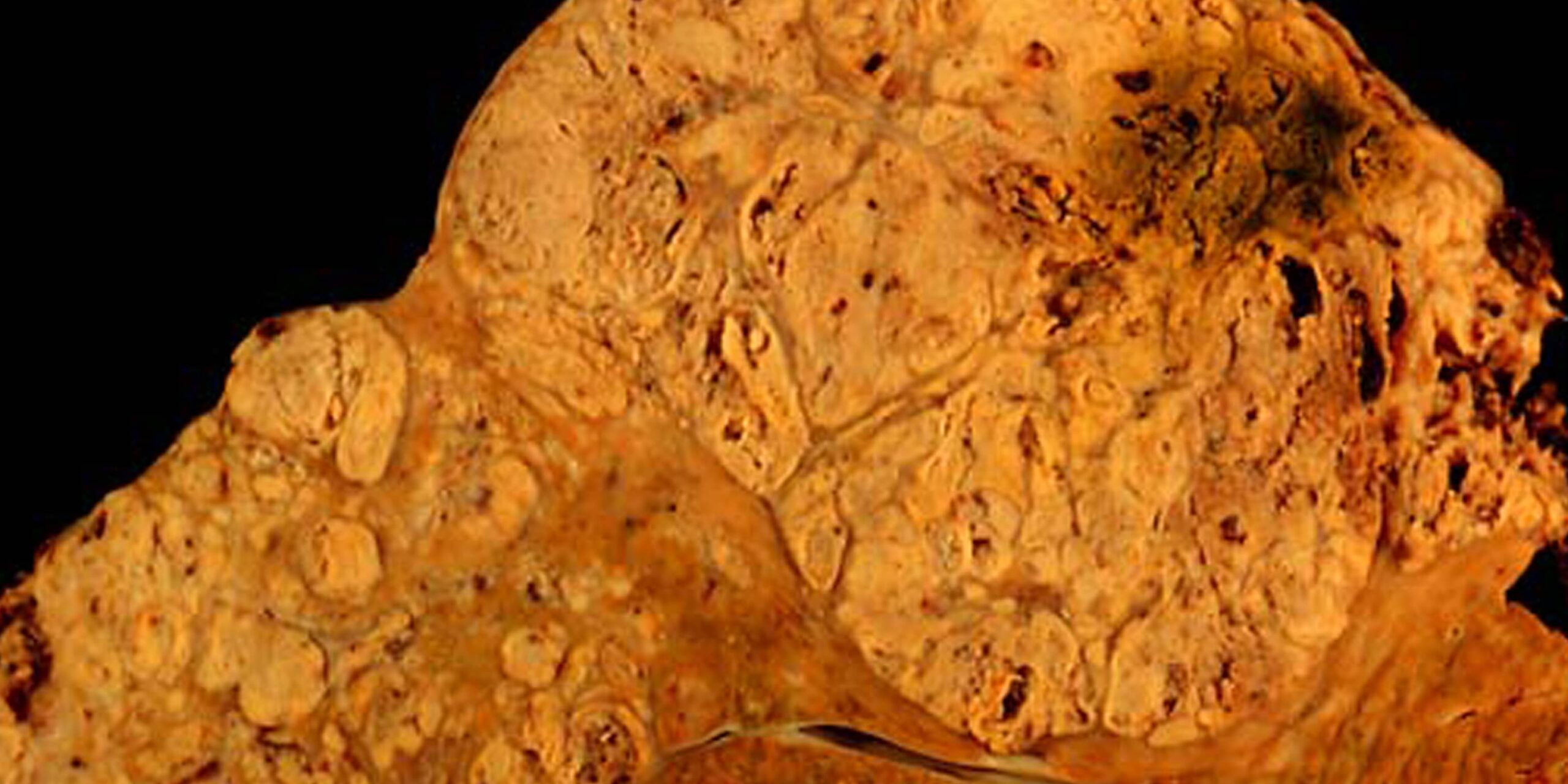
Hepatocellular carcinoma in a patient with hepatitis C
Risk factors
Several factors may favour the development of this cancer:
- pre-existing liver disease
- hepatitis B and/or C viruses
- alcohol
- overweight associated with diabetes
- hemochromatosis
Symptoms
When hepatocellular carcinoma (HCC) is in the early stages of the disease, it is usually asymptomatic and develops on top of existing liver disease: two diseases must therefore be managed, a cancer and a precancerous state.
As the disease progresses, the following signs may appear:
- pain in the abdomen,
- a palpable mass due to the tumor (usually under the ribs),
- jaundice – an increase in bilirubin levels in the blood and skin,
- weight loss,
- fatigue,
- digestive problems – digestion can be difficult and painful,
- changes in intestinal transit (diarrhea, constipation),
- discomfort,
- heavy legs and swollen feet (edema),
- hepatic encephalopathy,
- portal hypertension.
Generally speaking, one of the most common signs is a disturbance in the blood balance resulting from abnormal liver function.
Diagnosis and management
Hepatocellular carcinoma is an asymptomatic cancer in its early stages, often associated with chronic liver disease.
This cancer may be discovered following a surveillance examination, or by chance during a routine visit
In case of suspicion, there are various diagnostic tools available:
- palpation of the liver by a physician,
- a blood test for alpha-feto-protein (AFP), a tumor marker specific to hepatocellular carcinoma,
- a radiological examination (ultrasound, CT scan, MRI),
- if there is any doubt, a biopsy may be taken to establish an anatomopathological diagnosis of the cancer.
Treatment – Post-operative follow-up
Patient cases are discussed at multidisciplinary consultation meetings held once a week at Strasbourg’s NHC (Nouvel Hôpital Civil). The aim of these meetings is to establish the best therapeutic protocol for patients being treated for cancer. This means that the patient’s treatment is not decided by a single doctor, but by a multidisciplinary team of doctors.
Treatment of hepatocellular carcinoma must take into account the severity of the underlying liver disease, the patient’s general condition, the presence of metastases outside the liver, and the location and size of the tumor. It will also be necessary to treat the chronic disease that has caused the liver cancer to progress.
Treatment options will be discussed according to the stage and severity of the disease.
Different therapies may be used, such as :
- Surgical liver resection therapy
Hepatic resections are proposed for the treatment of single, small nodules.
Hepatectomies can be performed by laparotomy, laparoscopy or robotic-assisted surgery.
This type of treatment requires a hospital stay of around 7 days.
The minimally invasive approach may allow a very short stay (1-2 days). - Chemoembolization
Direct intra-arterial injection into the nodule under radiological control.
This type of treatment requires a hospital stay of around 3 days. - Local destruction or radiofrequency
Local destruction therapies are used for lesions that are difficult to access surgically, or in subjects with severely impaired liver function. Under radiological control (CT scan or ultrasound), a needle is inserted percutaneously into the lesion and treated by passing energy through the nodule, either by radiofrequency or microwave.
This type of treatment requires an average hospital stay of 2 to 3 days. - Radiotherapy
This technique is an alternative to local destruction if the HCC is > 3cm in size, especially if the tumor is located in the upper part of the liver.
Several sessions are required during treatment. - Chemotherapy
Chemotherapy can be administered intravenously, and is recommended in cases of advanced disease.
Oral chemotherapy may also be considered. New drugs are currently being tested for patients with advanced disease. - Liver transplantation
After careful selection, liver transplantation may be an option.
Useful information
Download guide: Liver cancer treatments
by National Cancer Institute, e-cancer.fr
Cancer Info Line
Support throughout your care pathway
Quality patient care is an essential objective, and the patient is at the heart of our concerns.