Hepatobiliary and Pancreatic Unit
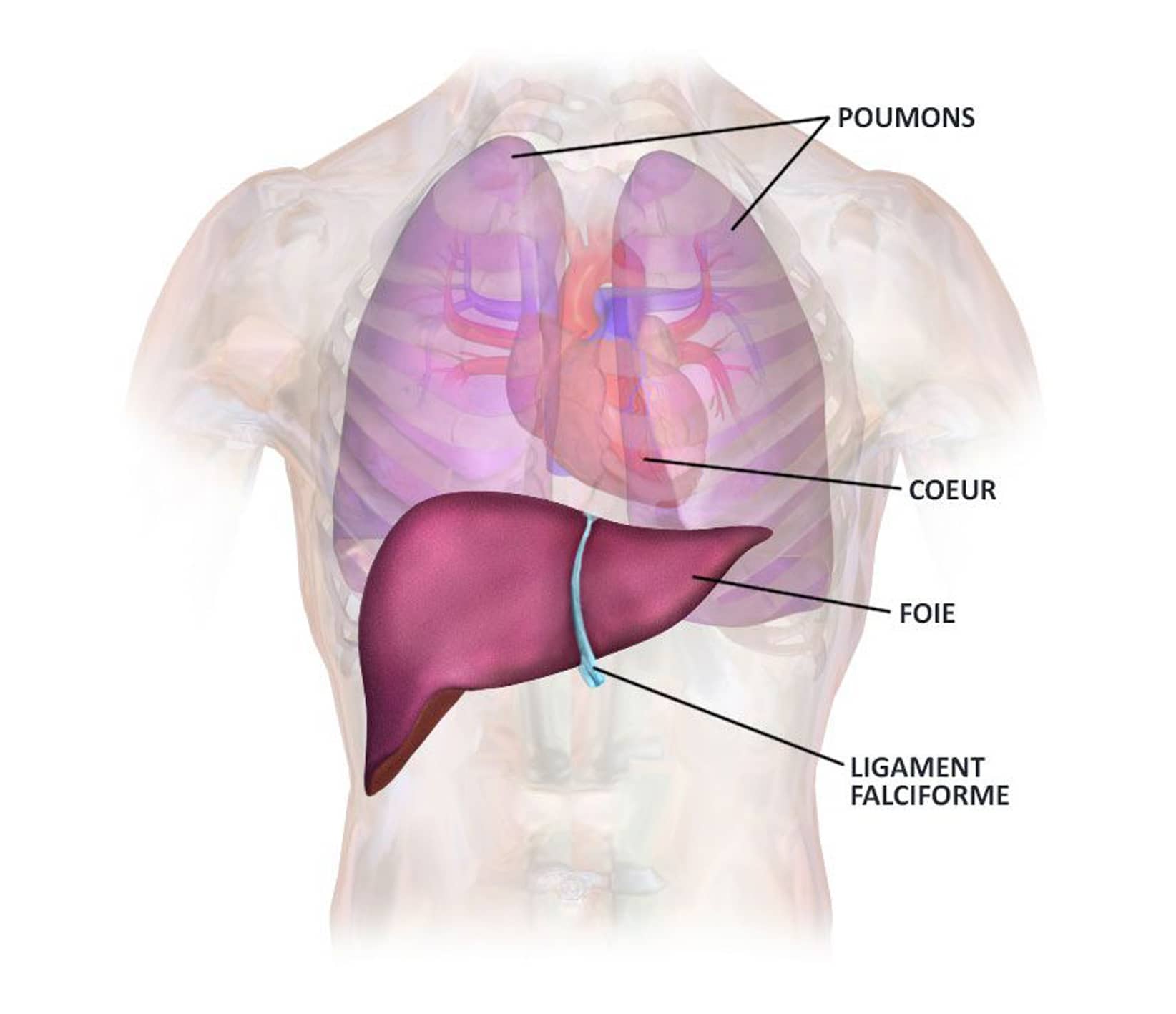
Liver anatomy
The liver is a unique abdominal organ, indispensable for life. To date, there is no way of artificially and permanently replacing its function.
It lies beneath the diaphragm, in the upper right-hand part of the abdominal cavity, and above the stomach, partly covering it. On average, it measures 28 cm wide, 16 cm high and 8 cm thick. Its own weight is approximately 1.5 kg.
The liver is a highly vascularized organ, and like the kidney, it is a great “blood cleaner”, metabolizing and neutralizing many of the toxic substances stored by the body.
The liver is a complex organ capable of remarkable regeneration, even if 3/4 of its mass has been resected or destroyed.
Cholangiocarcinoma (CC)
Cholangiocarcinomas are primary liver tumors that develop from the epithelium of the bile ducts. They can lead to obstruction of the bile ducts, resulting in impaired liver function and increased bilirubin, with jaundice, itching and abdominal pain. In many cases, the patient’s general condition is altered, with significant weight loss.
There are around 2,000 new cases of cholangiocarcinoma per year in France.
The location in the biliary tree allows us to identify three categories of tumors:
- Intrahepatic cholangiocarcinoma (tumor inside the liver)
- Extrahepatic cholangiocarcinoma (tumor outside the liver)
- Gallbladder cancer
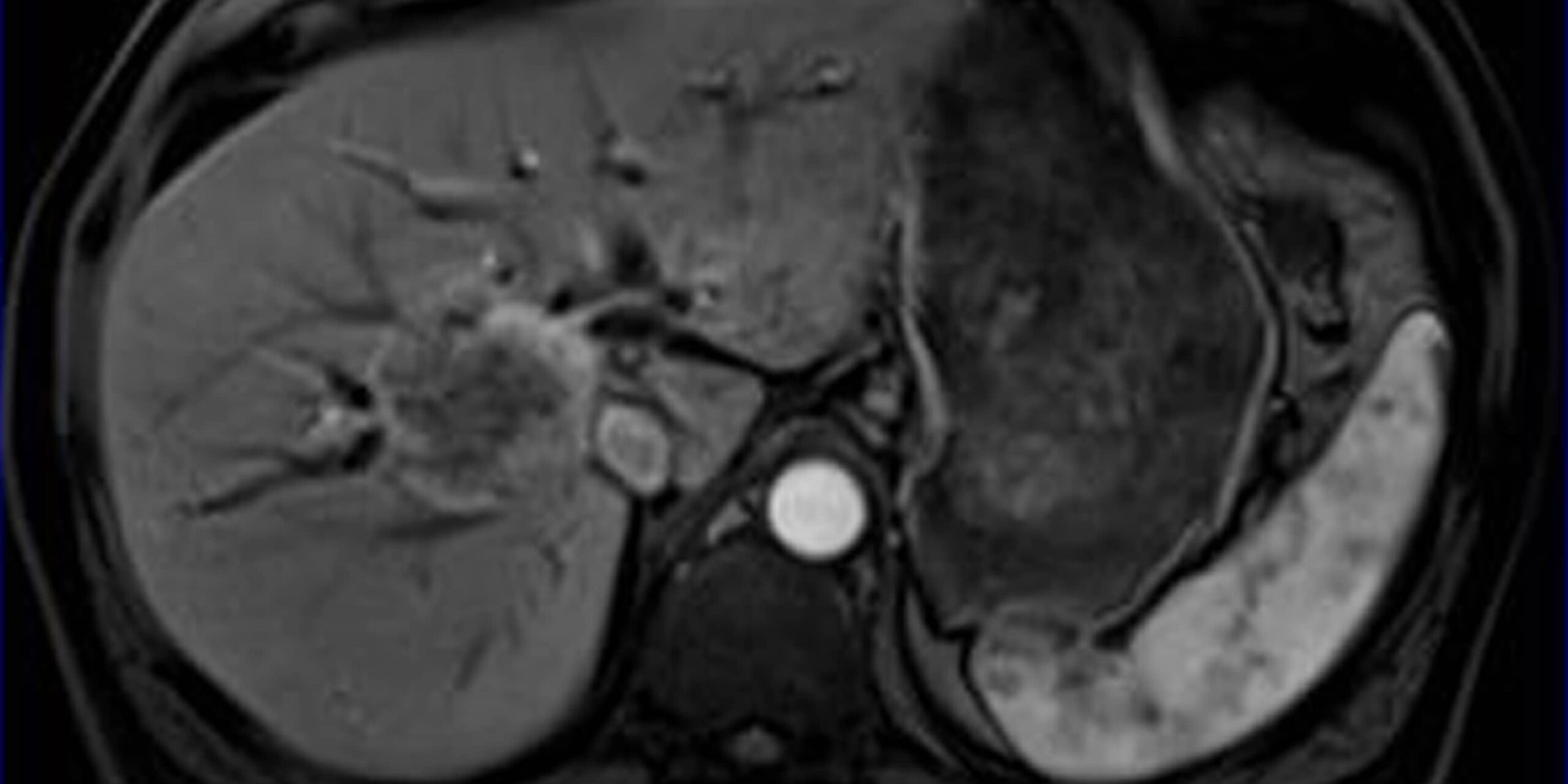
MRI showing cholangiocarcinoma, IHU Strasbourg
Risk factors
Several factors may favour the appearance of this cancer:
- age >65
- obesity
- type 2 diabetes
- inflammatory diseases:
- primary sclerosing cholangitis
- hepatolithiasis (eastern cholangiohepatitis)
- gallstones (biliary lithiasis)
- biliary-enteric anastomosis
- liver cirrhosis
- infectious diseases :
- opisthorchiosis – Opisthorchis viverrini (liver fluke)
- clonorchis sinensis (Chinese fluke)
- hepatitis B and C viruses
- HIV infection
- alcohol
- tobacco
- congenital diseases
- choledochal cyst
- Caroli disease
Symptoms
Symptoms can vary, depending on the location of the tumor (extrahepatic bile duct tumor, or intrahepatic bile duct tumor).
Generally speaking, one of the most frequent signs is a disturbance of the blood balance, due to abnormal liver function or to compression of the tumor on the internal structures of the liver.
As the disease progresses, the following signs may appear:
- jaundice – an increase in bilirubin levels in the blood and skin
This jaundice may be accompanied by itching - abdominal pain
- a change in stool color (discoloration due to the absence of bile salts in the digestive tract)
- darker, more colorful urine
- altered general condition
- fatigue
- weight loss
- loss of appetite
- and, in some cases, a rise in body temperature with fever
A blood test with liver function analysis (bilirubin, ASAT, ALAT, alkaline phosphatase and GT) reveals abnormalities.
Diagnosis and management
Cholangiocarcinoma is most often diagnosed following tumor biopsy. Characteristic signs on imaging frequently point to the diagnosis. Disturbed liver function tests and blood tests may indicate a biliary obstruction. Blood levels of Ca 19.9 and carcinoembryonic antigen (CEA) may be useful in suggesting a diagnosis of cholangiocarcinoma.
Imaging of the liver and bile ducts is necessary to assess the degree of disease. CT and MRI scans with specific biliary-MRI sequences provide valuable diagnostic information.
ERCP (endoscopic retrograde cholangio-pancreatography) may enable brushing for cytological examination, biopsy or prosthesis placement to temporarily resolve jaundice and biliary tract infection (angiocholitis).
If endoscopic treatment is not feasible, percutaneous external biliary drainage can be performed under radiological guidance.
Treatment – Post-operative follow-up
Patients suffering from cholangiocarcinoma are discussed at multidisciplinary consultation meetings held once a week at Strasbourg’s NHC (Nouvel Hôpital Civil). The aim of these meetings is to establish the best treatment protocol for patients undergoing treatment for this cancer. This means that the patient’s treatment is not decided by a single doctor, but by a multidisciplinary team of doctors
- Surgical resection
Surgical resection is the curative treatment for cholangiocarcinoma. The choice of surgery and type of resection is made following a full extension workup, and assessment of the liver reserve by calculating the volume of the remaining liver using specific software. The aim of surgery is to achieve complete resection. - Liver transplantation
Cholangiocarcinoma is usually a contraindication to liver transplantation. - Locoregional treatments
The value of external radiotherapy in patients with inoperable CC has not been clearly established.
With regard to transarterial chemoembolization and radioembolization, unlike for HCC, there are few data available on these treatments for cholangiocarcinoma, which are classically poorly vascularized tumors.
- Systemic therapies
Numerous systemic chemotherapies and combinations of chemotherapies have been studied, demonstrating a survival benefit of chemotherapy over supportive care.
After surgical resection, adjuvant treatment with oral chemotherapy is now proposed.
Useful information
Download guide: Liver cancer treatments
by National Cancer Institute, e-cancer.fr
Cancer Info Line
Support throughout your care pathway
Quality patient care is an essential objective, and the patient is at the heart of our concerns.