Hepatobiliary and Pancreatic Unit
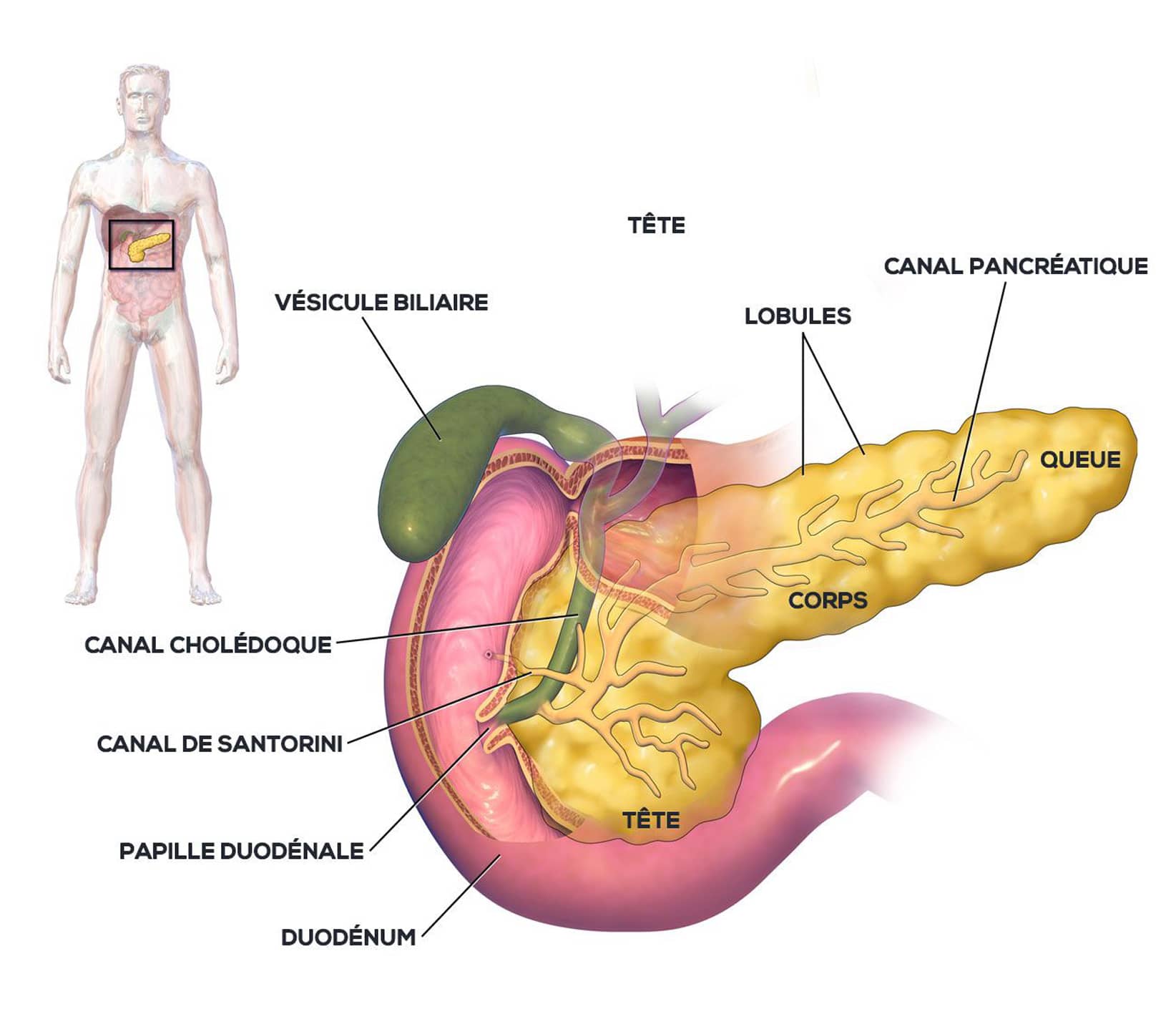
Anatomy of the pancreas
The pancreas is a visceral organ located in the abdomen, in the retroperitoneum, in front of the aorta and inferior vena cava, and behind the stomach. It is a gland of the digestive system.
The pancreas is the second largest gland after the liver.
Pale pink in color, the pancreas is normally soft and granular in appearance. It measures between 12 and 15 cm in adults and weighs approximately 80g. Its thickness decreases from right to left. The pancreas is divided into three parts, from its medial end to its lateral end: the head, the body and the tail.
The pancreas produces enzyme-rich secretions, which are discharged into the duodenum to aid digestion (exocrine function), and hormones, including insulin, which are discharged into the bloodstream to help regulate blood sugar levels (endocrine function).
Acute pancreatitis
Acute pancreatitis is an inflammatory disease of the pancreas that can lead to necrosis. The pancreas self-digests with its own enzymes, leading to necrosis. This destruction can lead to infection and multi-organ failure (liver, kidney, heart).
In the most severe cases, surgery may be required, and it usually takes several operations to stop the disease progressing.
This pathology can have serious complications, with a high mortality rate.
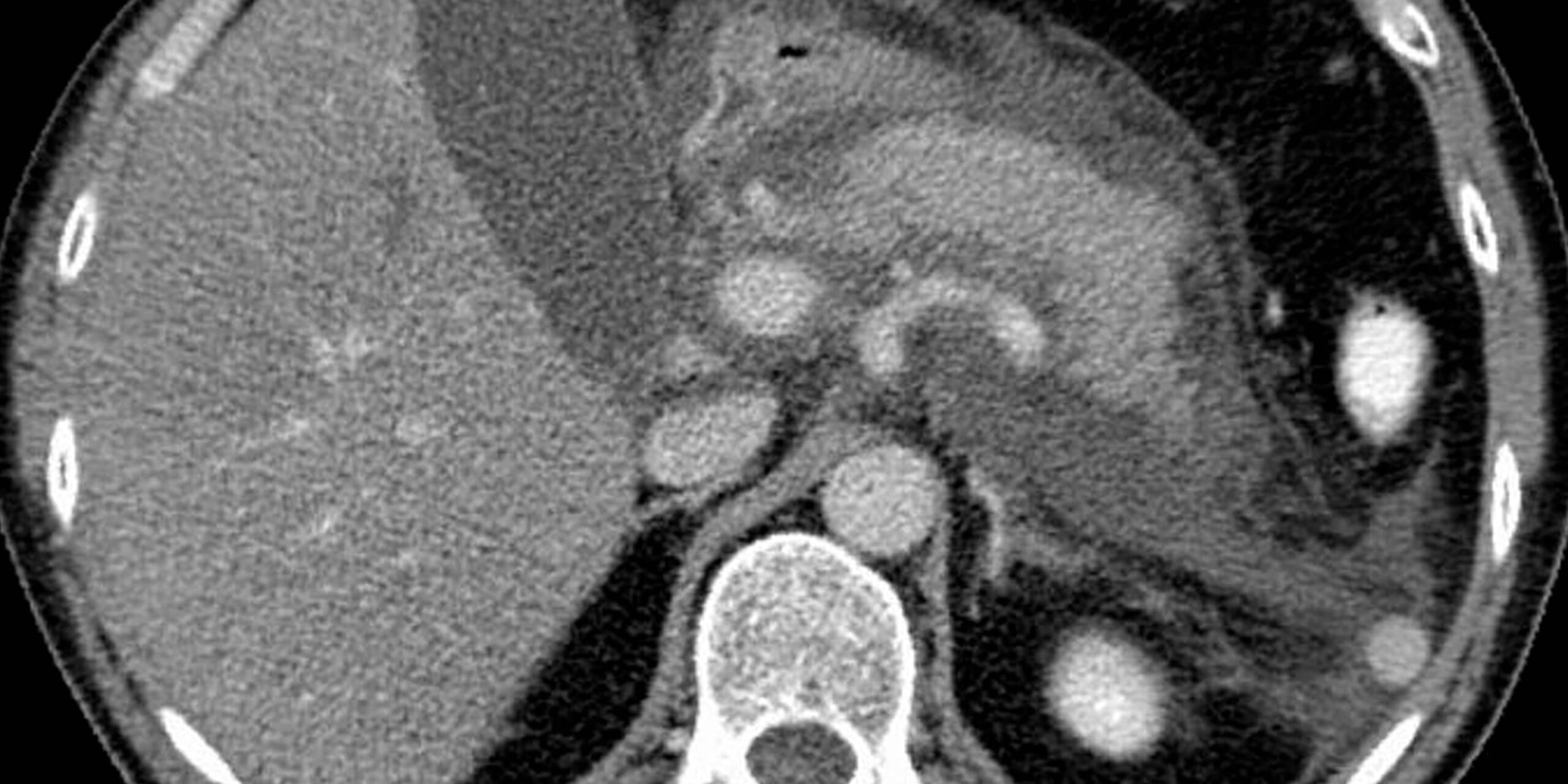
Patient with acute exudative pancreatic disease with pockets of fluid surrounding the pancreas, Wikimedia Commons
Risk factors
Several factors can contribute to the onset of this disease:
- excessive alcohol consumption or sudden, heavy alcohol abuse
- a mechanical origin linked to obstruction of the bile ducts by gallstones
- chronic pancreatic disease
- mumps
- metabolic origin
- drug-induced
- viral, parasitic or bacterial infection
- hereditary origin
A few rare cases of acute pancreatitis have no known cause.
Symptoms
The patient presents with sudden, almost constant pain, which may also be accompanied by:
- pain radiating to the back,
- the patient is often bent over,
- frequent nausea and vomiting,
- bloating,
- pale, icy hands and feet,
- a rise in body temperature with fever.
Diagnosis and management
Diagnosis is based on clinical examination and blood levels of pancreatic enzymes such as lipase.
An abdominal CT scan is the gold standard (within 48 hours of the onset of symptoms) for the immediate management of acute pancreatitis, as it provides an accurate picture of the lesions. To determine the cause of the pancreatitis, hepato-biliary ultrasound, Bili-MRI and/or echo-endoscopy of the pancreas may be performed.
Treatment – Post-operative follow-up
The disease can be cured quickly and not be serious, but it can also be serious or fatal, requiring hospitalization for varying lengths of time.
Acute pancreatitis is said to be “severe” if there is organ failure or a local complication.
One case in five is said to be “severe”.
A range of therapies are available, including:
- Conventional drug treatment:
Treatment of acute pancreatitis often requires hospitalization, with the patient fasting (with intravenous nutrition) to rest the pancreas. Pain is also treated with analgesics (morphine if necessary). In the event of complications, surgery is required. - Drainage of infected collections may be necessary, and is preferably performed by endoscopy or percutaneous radiology.
Surgery is only an option when other treatments have failed.
The cause of the pathology must also be identified and treated to eliminate any risk factors for recurrence.
Useful information
Download guide: Pancreatic cancer treatments
by National Cancer Institute, e-cancer.fr
Cancer Info Line
Support throughout your care pathway
Quality patient care is an essential objective, and the patient is at the heart of our concerns.