Hepatobiliary and Pancreatic Unit
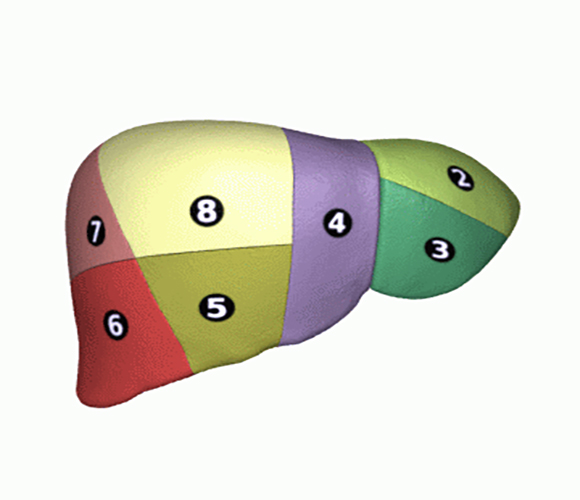
Liver segmentation (Couinaud), Wikimedia Commons
Minor hepatectomy
The principle of a hepatectomy consists of removing part of the liver, thus removing malignant or benign lesions of the liver. The lesions can be primary (directly from the liver) or secondary, i.e. metastases.
For all hepatectomies, the choice of the minimally invasive or classic open operating method is discussed and depends on several factors (the location of the lesions, the general state of health of the patient, etc.).
In the case of a minimally invasive operating method (laparoscopy or robot-assisted), the patient in the operating room is prepared with the installation of trocars which will be used to insert the various tools necessary for the operation.
By definition, a minor hepatectomy involves less than 3 segments. It is an intervention which resects a small part of the liver by removing in one piece the area which contains the liver cancer with the section of its venous, arterial and biliary pedicles.
Hepatectomy is a technical and delicate surgical procedure.
Before the intervention
THE CONSULTATION WITH THE SURGEON
Before a hepatectomy, the patient undergoes various examinations to determine the type of liver injury, and to determine the overall function of the liver and its volume to allow planning of the intervention and its risks.
IHU Strasbourg benefits from the latest technological advances in diagnostic imaging tools such as: ultrasound, CT or scanner, MRI, angiography, 3D reconstruction imaging, etc. The result of these images makes it possible to create a three-dimensional model of the patient’s organ, thus obtaining an identical reconstruction which allows personalized solutions to be defined. In special cases, during the operation, the surgeon can use the 3D reconstruction which is accurately superimposed on the patient’s body (augmented reality).
With the results obtained, the surgeon indicates to the patient the objectives of the operation, the technique used and the possible postoperative consequences and complications.
THE CONSULTATION WITH THE ANESTHETIST
Hepatectomy is performed under general anesthesia.
This consultation allows the risks associated with anesthesia to be assessed, taking into account medical, family and surgical history. It is very important to report any health problems (allergies, respiratory and heart problems, medication treatment, alcohol and tobacco consumption). In general, it is strongly recommended to stop drinking alcohol and tobacco a few weeks before the procedure.

Features
The transection can be performed with clamping of the hepatic pedicle to reduce bleeding.
Procedure
Hepatectomy can be performed by different surgical techniques such as laparotomy, laparoscopy and robotic-assisted surgery.
The operating time is approximately 3 hours.
The length of hospitalization is approximately 5 days.
These durations are based on an approximation, they may be longer depending on the patient’s state of health.
Benefits and advantages
Hepatectomy is the only intervention that can guarantee the patient’s long-term survival in the event of malignant liver lesions. The liver has the ability to regenerate itself, if the liver tissue is healthy, and to reconstitute itself to its entire normal mass. If the hepatectomy is total (total removal of the liver), it will precede a liver transplant.
Risks and complications
The main risks are hemorrhage with the need for transfusion, leakage of bile on the cut edge of the liver and, to a lesser extent, liver failure.
Useful information
Download guide: Liver cancer treatments
by National Cancer Institute, e-cancer.fr
Cancer Info Line
Support throughout your care pathway
Quality patient care is an essential objective, and the patient is at the heart of our concerns.