Hepatobiliary and Pancreatic Unit
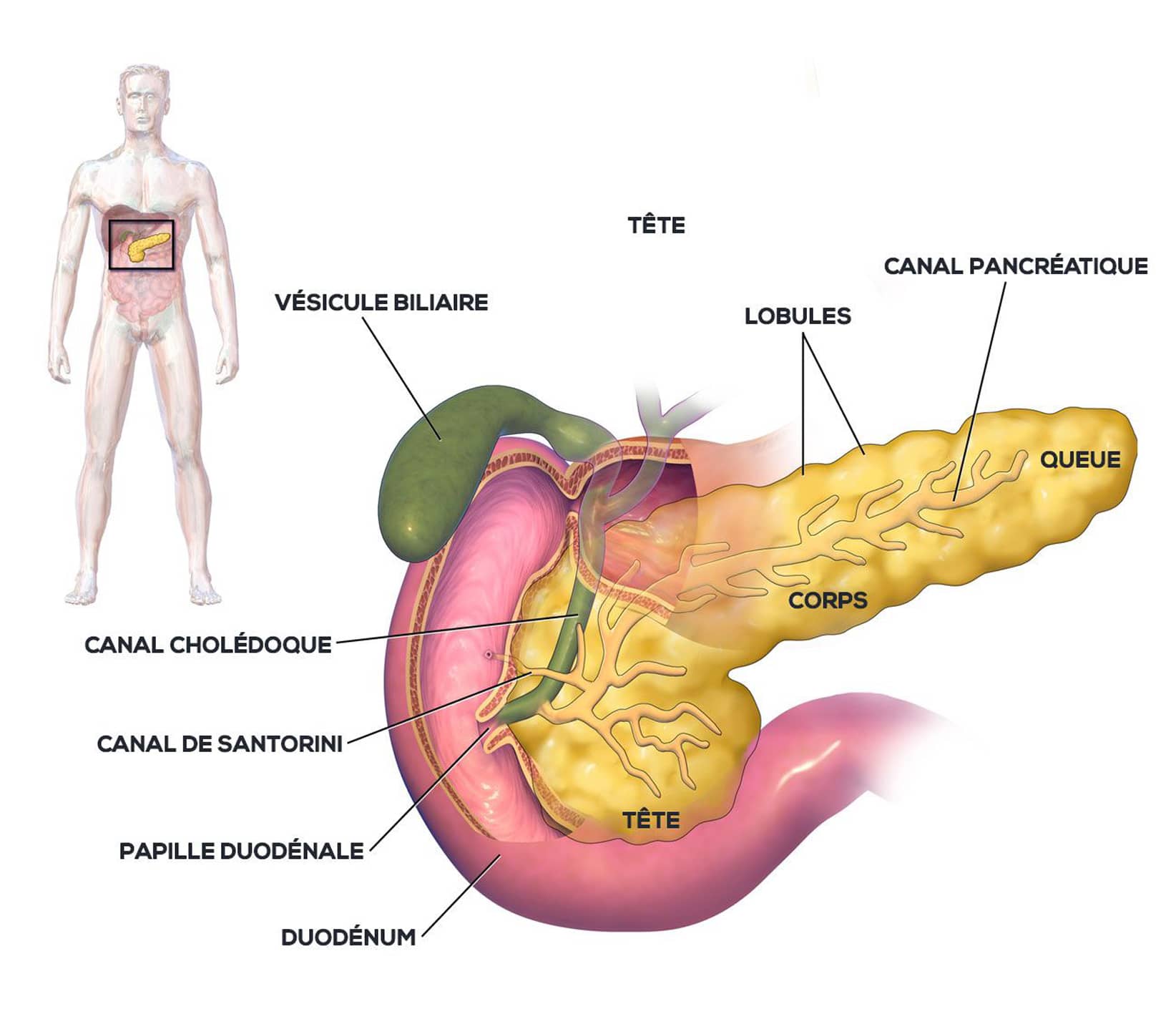
Pancreas: Left pancreatectomy (± spleen)
This intervention consists of removing the left part of the pancreas, that is to say the body and tail of the pancreas. It possibly includes removal of the spleen (splenectomy) depending on vascular invasion and the need to remove the lymph nodes (lymph node dissection).
Left pancreatectomy may be indicated for patients suffering from chronic pancreatitis, cystic tumors, benign or malignant tumors and pancreatic trauma.
Before the intervention
THE CONSULTATION WITH THE SURGEON
Before a pancreatectomy, the patient undergoes various examinations to determine the type of pancreatic lesion and the indication for surgical treatment.
IHU Strasbourg benefits from the latest technological advances in diagnostic imaging tools such as: ultrasound, CT or scanner, MRI, angiography, 3D reconstruction imaging, etc. The result of these images makes it possible to create a three-dimensional model of the patient’s organ, thus obtaining an identical reconstruction which allows personalized solutions to be defined.
With the results obtained, the surgeon indicates to the patient the objectives of the operation, the technique used and the possible postoperative consequences and complications.
THE CONSULTATION WITH THE ANESTHESIST
Pancreatectomy is performed under general anesthesia.
This consultation allows the risks associated with anesthesia to be assessed, taking into account medical, family and surgical history. It is very important to report any health problems (allergies, respiratory and heart problems, medication treatment, alcohol and tobacco consumption). In general, it is strongly recommended to stop drinking alcohol and tobacco a few weeks before the procedure.

Features
This procedure does not require digestive or biliary reconstruction at the end of the operation.
It requires single-piece ablation of the area containing the lesion without altering digestive continuity.
Procedure
Pancreatectomy can be performed by different surgical techniques such as laparotomy, laparoscopy and robotic-assisted surgery, it requires general anesthesia.
The operating time is approximately 4 hours and the hospital stay is approximately 7 days.
Benefits and advantages
Pancreatectomy is the only procedure that can guarantee long-term survival in cases of malignant pancreatic tumors.
Risks and complications
The main post-operative risks are:
- Leak at the pancreatic section area (pancreatic fistula)
- Post-operative hemorrhage
- In the medium and long term, the occurrence of diabetes
If the spleen is removed at the same time, vaccination against pneumococcus, meningococcus, and Haemophilus will be recommended with antibiotic therapy with penicillin for 2 years after the operation.
Mortality linked to the intervention is <1%.
useful information
Download guide: Pancreatic cancer treatments
by National Cancer Institute, e-cancer.fr
Cancer Info Line
Support throughout your care pathway
Quality patient care is an essential objective, and the patient is at the heart of our concerns.